What is CAQH? A Guide for Behavioral Health Therapists

If you are a therapist accepting Medicaid or insurance, you likely have heard about CAQH from the credentialing process. Whether you’re new to insurance-based practice or looking to streamline your administrative tasks, understanding CAQH credentialing is essential. Behavioral health professionals simply must grasp the function of CAQH to manage provider information and work with private insurance.
In this guide, we will break down:
- What CAQH ProView is
- Its role in the credentialing process
- What documents you’ll need
- How to navigate this platform as a CAQH provider
What is CAQH?
CAQH (Council for Affordable Quality Healthcare) is a nonprofit organization that helps simplify the administrative processes between healthcare providers and insurance companies. Its primary purpose is to reduce paperwork and streamline credentialing for healthcare professionals, including mental health professionals.
The CAQH ProView platform serves as a centralized database where providers can submit and maintain professional and practice information. Insurance companies then access this information to verify a provider’s credentials and approve them to join their network.
History of CAQH
In 1999, a coalition of health plans and healthcare providers founded CAQH to improve administrative efficiency. The launch of CAQH ProView (formerly CAQH Universal Provider Datasource) in 2002 marked a significant shift toward electronic credentialing.
Over the years, CAQH ProView has become the industry standard for provider data collection and sharing. There have been more than 1.6 million healthcare providers using the platform as of 2024 (CAQH).
Why is CAQH Important for Therapists Accepting Insurance?
If you plan to accept Medicaid or private insurance, most payers will require you to credential through CAQH. The platform is a digital app that many insurance companies can use. It makes it easier to share your information, and you won’t need to submit separate applications to each company.
Many insurance panels — including Blue Cross Blue Shield, UnitedHealthcare, Aetna, and Medicaid programs — rely on CAQH to verify providers. Without a CAQH profile, you might experience delays or denials in your credentialing applications.
How to Create a CAQH ProView Profile
Setting up your CAQH ProView profile is a critical step in becoming an in-network provider. Here’s how the process works:
Register with CAQH ProView
- Visit the CAQH ProView website: https://proview.caqh.org
- Create an account and select your provider type (Mental Health Therapist, LCSW, LPC, LMFT, etc.).
Complete Your Profile
- Fill out personal and professional information, including:
- Contact details
- Education and training
- Licensure
- Practice locations
- Insurance coverage
- Work history
- Malpractice history
Upload Supporting Documents You’ll need to provide digital copies of the following documents:
- State license
- Liability insurance (malpractice coverage)
- W-9 tax form
- DEA certificate (if applicable)
- Board certifications
- Education diplomas
- Current CV or resume
Authorize Payers
- Grant permission for insurance companies to access your profile. Most payers will send you an invitation to authorize them in the CAQH system.
Attest to Your Information
- CAQH requires providers to re-attest their information every 120 days, ensuring that all data remains updated and accurate.
How Long Does CAQH Credentialing Take?
The timeline for CAQH credentialing depends on a few factors. It includes how fast you submit your information, as well as how long insurance companies take to verify documents. On average, the process takes 4-8 weeks, but it can take longer if there are errors in your application.
Is There a Cost for CAQH ProView?
Creating and maintaining your CAQH ProView profile is free for providers. However, some insurance companies may charge credentialing fees as part of their application process.
Tips for Maintaining Your CAQH Profile
- Keep Information Updated: Update your profile anytime you change your address, license status, or insurance coverage.
- Set Reminders for Attestation: CAQH sends reminders every 120 days, but setting personal alerts can help stay on track.
- Double-Check Documents: Ensure that all documents are legible, current, and properly labeled before uploading.
- Respond to payer invitations quickly. The sooner you show your profile to insurance companies, the faster they can begin the credentialing process.
Common Mistakes to Avoid
- Uploading expired documents
- Incomplete work history
- Forgetting to re-attest
- Not authorizing payers
- Using inconsistent information across different applications
How CAQH Fits into Medicaid Credentialing
If you’re applying to become a Medicaid provider, most state Medicaid programs require a CAQH profile to start. Be sure to check with your state Medicaid office for any additional requirements or application steps.
Final Thoughts
Navigating CAQH credentialing can be overwhelming. This is especially true for mental health therapists starting accepting insurance. Creating and keeping your CAQH ProView profile is an important step. It helps you become an in-network provider and it makes your mental health services easier for clients to access.
By staying organized and keeping your profile updated, you can make the credentialing process easier. This lets you focus on what matters most: providing quality care to your clients.
For more helpful information on CAQH and insurance credentialing, check out these resources:
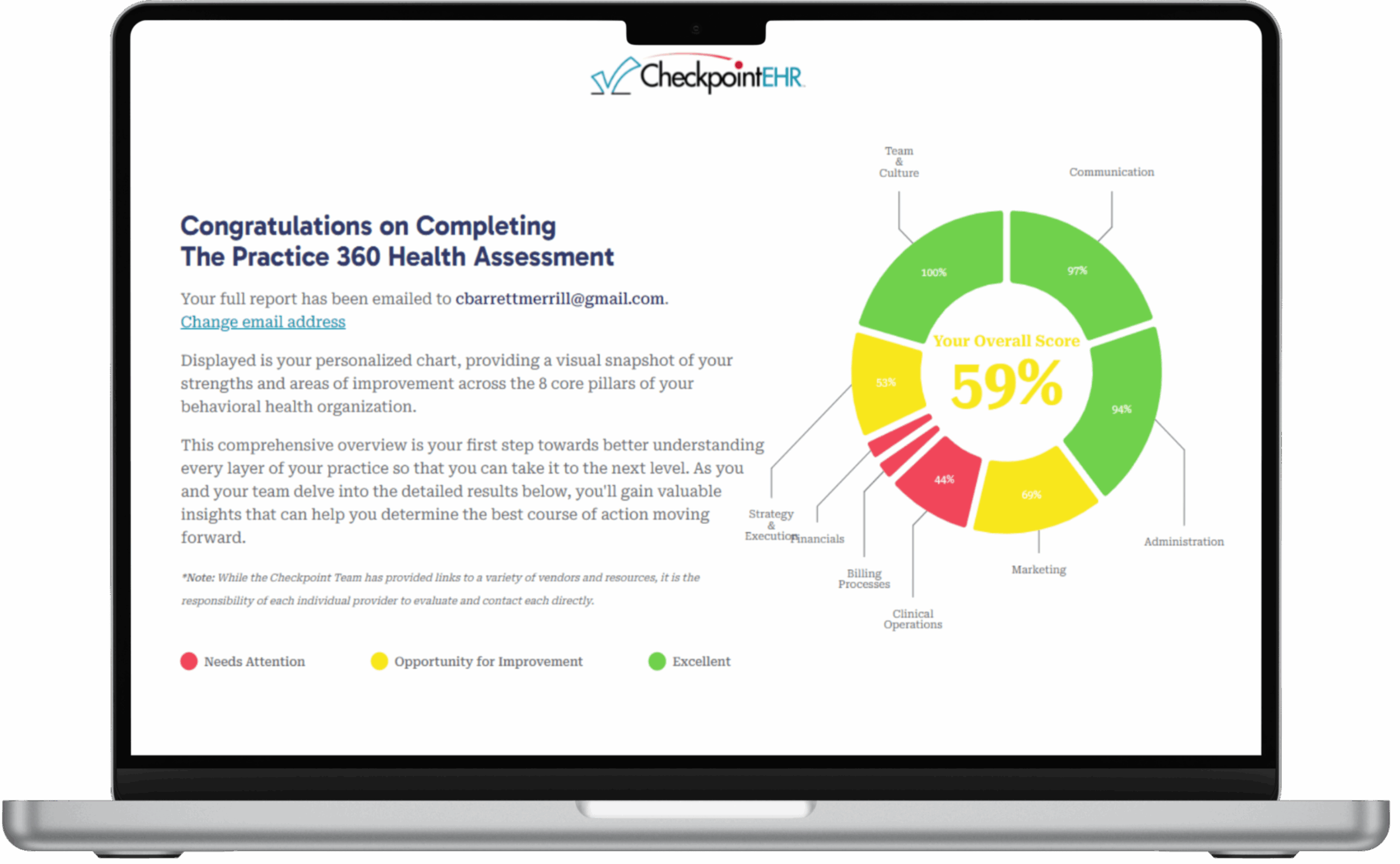
If you’re looking for a streamlined EHR platform that simplifies billing and claims management, CheckpointEHR is the tool for you. You can learn more about our intuitive and efficient EHR software here.