Join the Best Practice Therapist newsletter today → Subscribe
Authorization Tracking
Track client authorization with easy-to-use unit monitoring and automated alerts, ensuring that clients are approved and covered for the services they are seeking.
Track Client Authorization with Payers
Avoid possible claims rejections and denials by staying on top of client authorization.
Unit Monitoring
Have granular insight into client coverage units with payers.
Key Date Notifications
Track all important dates around client coverage.
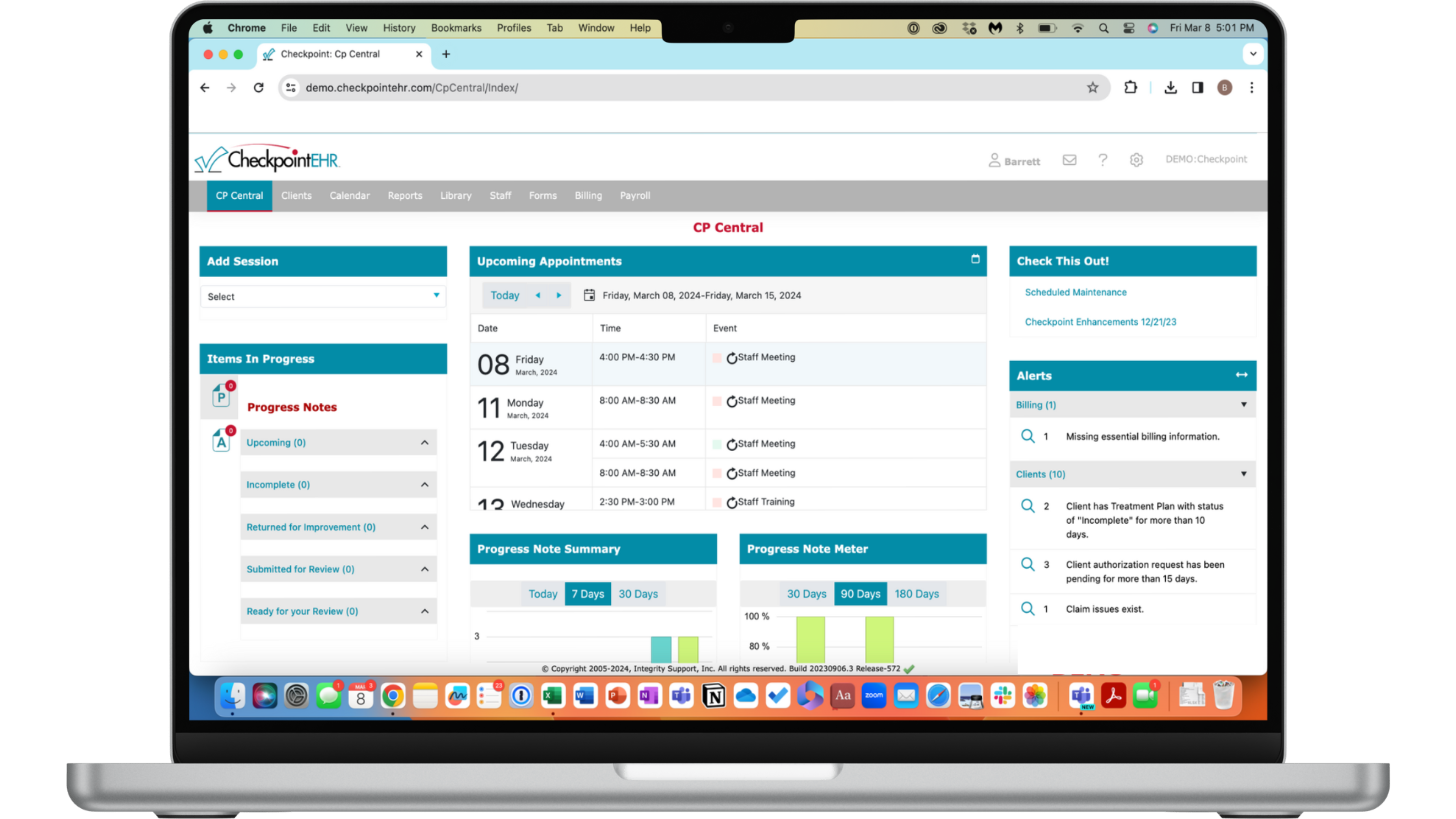
Dashboard Alerts
Receive dashboard alerts for any authorization errors.
Attachments
Securely store client authorization files.
Unit Monitoring
Track the exact amount of coverage units each client has under their plan with a specific payer, and monitor unit changes over time as services are provided.
Key Date Notifications
Log all important dates and time ranges for each client's care plan and payer coverage.
Dashboard Alerts
Receive dashboard and email alerts when there are any authorization issues with client or payer information, coverage units, or plan expiration dates.
Attachments
Securely store all files and documents pertaining to a client's coverage to track and log important information around their particular care plan and authorization.
Check out Janine's Story
See how Liaisons Wellness Center benefited from CheckpointEHR’s clinician-friendly EHR system in this case study.
What people are saying...
“You are a wonderful team. We have tried EHRs before with different companies and they were not able to deliver, but Checkpoint is diligent, faithful, responsive, and always there. It is greatly appreciated. The entire office staff loves working with Checkpoint. It has really prepared us for expansion. The assistance you give is wonderful.”
Tamika
Business Manager

Join the Best Practice Therapist Newsletter!
Free behavioral health tips & resources delivered straight to your inbox. From clinical operations and organizational management, to scaling your practice and digital marketing, Best Practice Therapist provides you with practical tools & insights in 1-2 minute doses.
Looking to evaulate a new EHR system for your practice?
Get in touch with us today to learn more!