The Importance of Tracking Outcome Measurements for Your Practice
In recent years, the healthcare industry has begun to adopt approaches used in other types of industries to improve the level of service provided to patients and to manage costs more effectively. One of the key strategies has been to track the effectiveness of various treatments by taking outcome measurements, and there are major benefits to tracking outcome measurements.
Better Cost Control
All efficient healthcare practices will have a dynamic strategy in place to reduce costs. However, without proper outcome measurement, cost-cutting initiatives can be self-defeating and may even result in increased costs. For example, making a decision to increase the time interval between patient callbacks for certain types of treatment will deliver short-term cost savings, but may result in significantly higher overheads in the long term.
Outcome measurements can help healthcare providers to identify the most effective treatments based on individual patient outcomes. Medical personnel understand that there is no “one size fits all” in dealing with individual health problems. Nevertheless, many medical staff will persistently rely on standard treatments because they have no system in place to measure outcomes. This can lead to unnecessary repeat patient visits, increased surgical revisions and overall patient dissatisfaction, all of which have cost implications.
Apart from reducing costs, using outcome measurements can also lead to an increase in income for a healthcare provider. By being able to fine-tune treatments based on outcomes, providers will often find that the improved efficiency enables them to take on more patients.
Improving the Patient Experience
In healthcare practices that are proactively patient-centric, improving the patient experience is a key goal. The patient experience can be vastly improved when a healthcare practice recognizes the importance of outcome measurements.
Healthcare providers who use outcome measurements will find it much easier to adapt treatments, resulting in a higher level of patient satisfaction. Outcomes can be measured in several different ways using a tier system, but it is important to take the patient’s own input into account when establishing what is considered a favorable outcome.1 From a clinical perspective, prolonging the life of a patient with terminal cancer may be considered a positive outcome. The patient, on the other hand, may feel that treatment which reduces their quality of life is a negative outcome.
Making Patients Better Informed
Measuring outcomes can help medical practices understand more from patients’ perspectives. The data accumulated from measuring outcomes can lead to better interactions with patients, and it can help medical personnel allow patients to have a more informed say in how they want to be treated, something that can be otherwise problematic.2
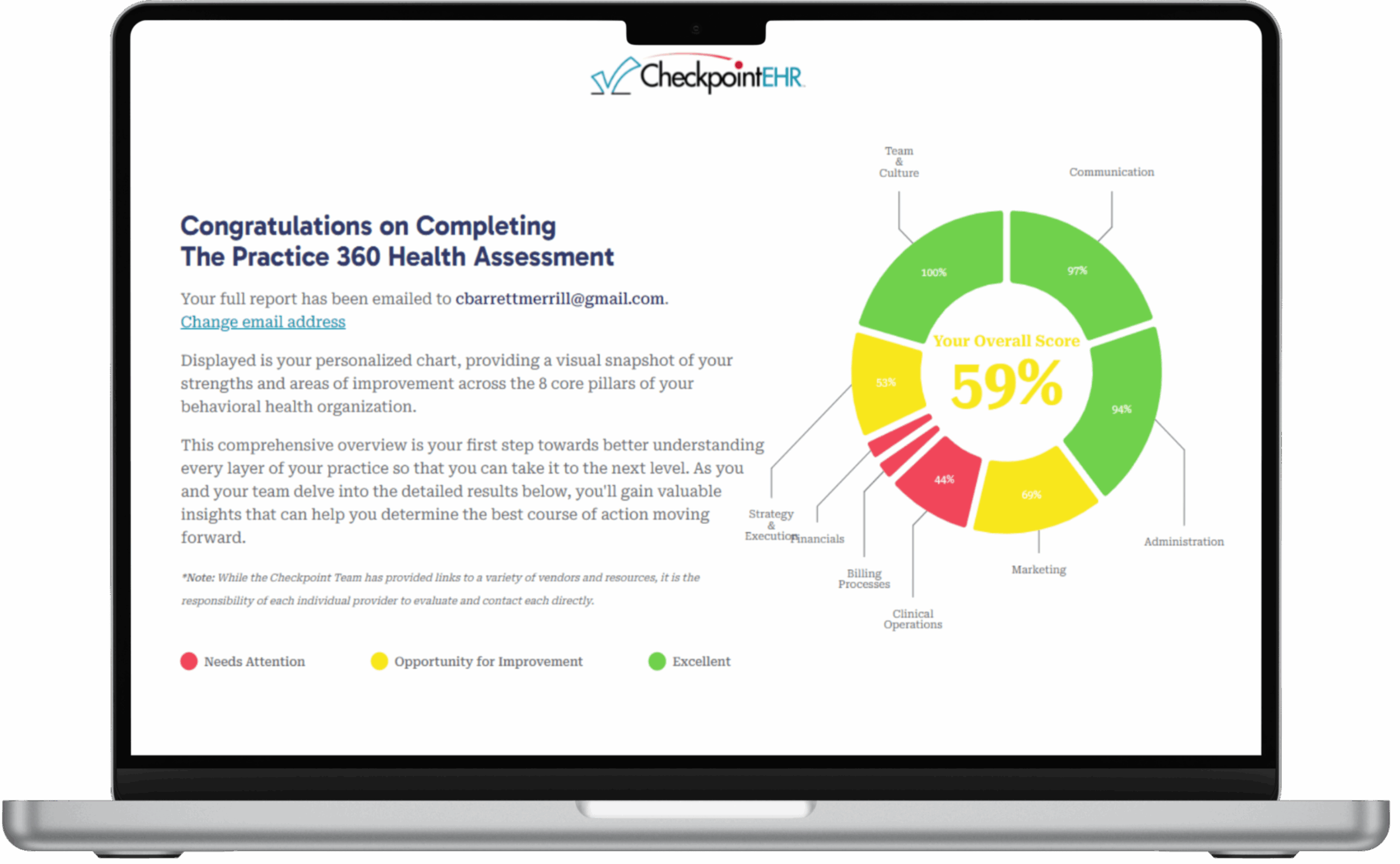
It is worth noting that there is an administrative overhead in measuring outcomes, but that can be significantly reduced by using efficient software tools. Many practices use their EHR systems, and the better systems, such as Checkpoint EHR, can help with measuring outcomes by providing easy-to-use tracking features. These, combined with graphic analyses tools, can let you see at a glance how effective your treatments are, and to respond quickly when results are less than satisfactory.