What is the Difference Between a Claim Rejection & a Claim Denial?
In the world of healthcare billing, there are plenty of terms that get mixed up easily. One question we repeatedly hear while working in the EHR (electronic healthcare records) and billing space is, “What is the difference between a claim rejection and a claim denial?” Some people may not even realize there is a difference between claim rejections and claims denials, but knowing the difference could save you time and money.
Neither a rejected nor a denied claim is going to be paid until it is somehow resubmitted with the right claim data in it. But the difference lies in at what point in the claim submission process the payer (the insurance) made that decision.
What is a claim rejection?
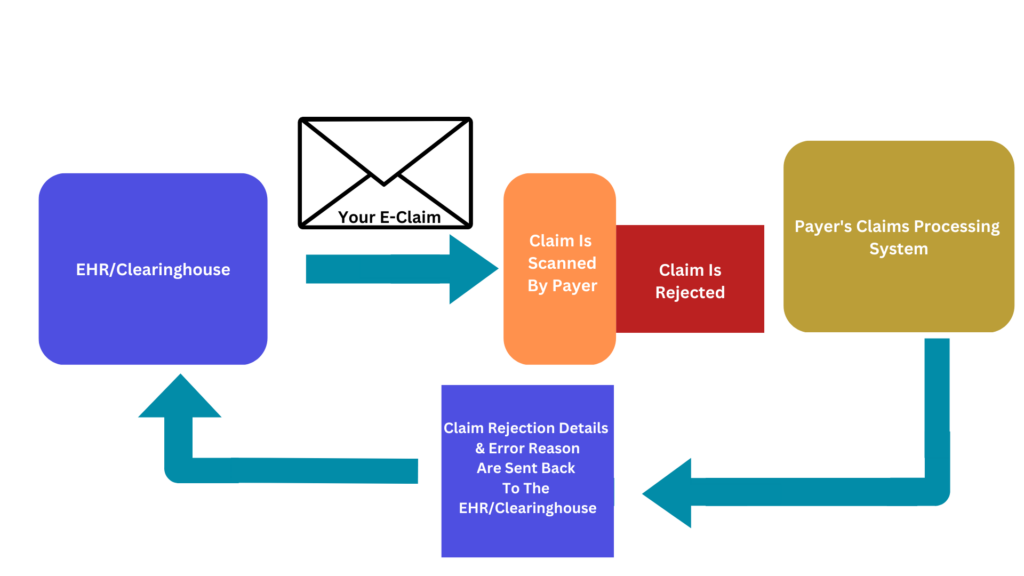
When a claim is rejected, the payer’s claims processing system reads the claim data and decides to block it from being processed; this means that there was not a claim number assigned to the claim, and if you were to call the payer’s claims department, they likely would say that they do not see a claim on file matching the information you give them. A claim rejection is often the answer when mental healthcare providers ask, “Why does the insurance/payer not have the claims I submitted?” When the claim is rejected, the payer will likely send an error reason for the rejected claim back to the system that the claim came from. In the case of Checkpoint EHR, our software has a page dedicated to helping mental healthcare providers keep track of and manage those claim rejections and display the error reasons. The good news about claim rejections is that they are usually easy to fix. Claim rejections are most commonly caused by the information on the claim not matching the information in the payer’s system (examples: misspelt client names, incorrect provider NPI numbers, incorrect client insurance identification numbers, etc.) Fixing a claim rejection is usually just fixing the incorrect information in your EHR system and submitting the claim again. The graphic above will help you visualize claim rejections.
What is a claim denial?
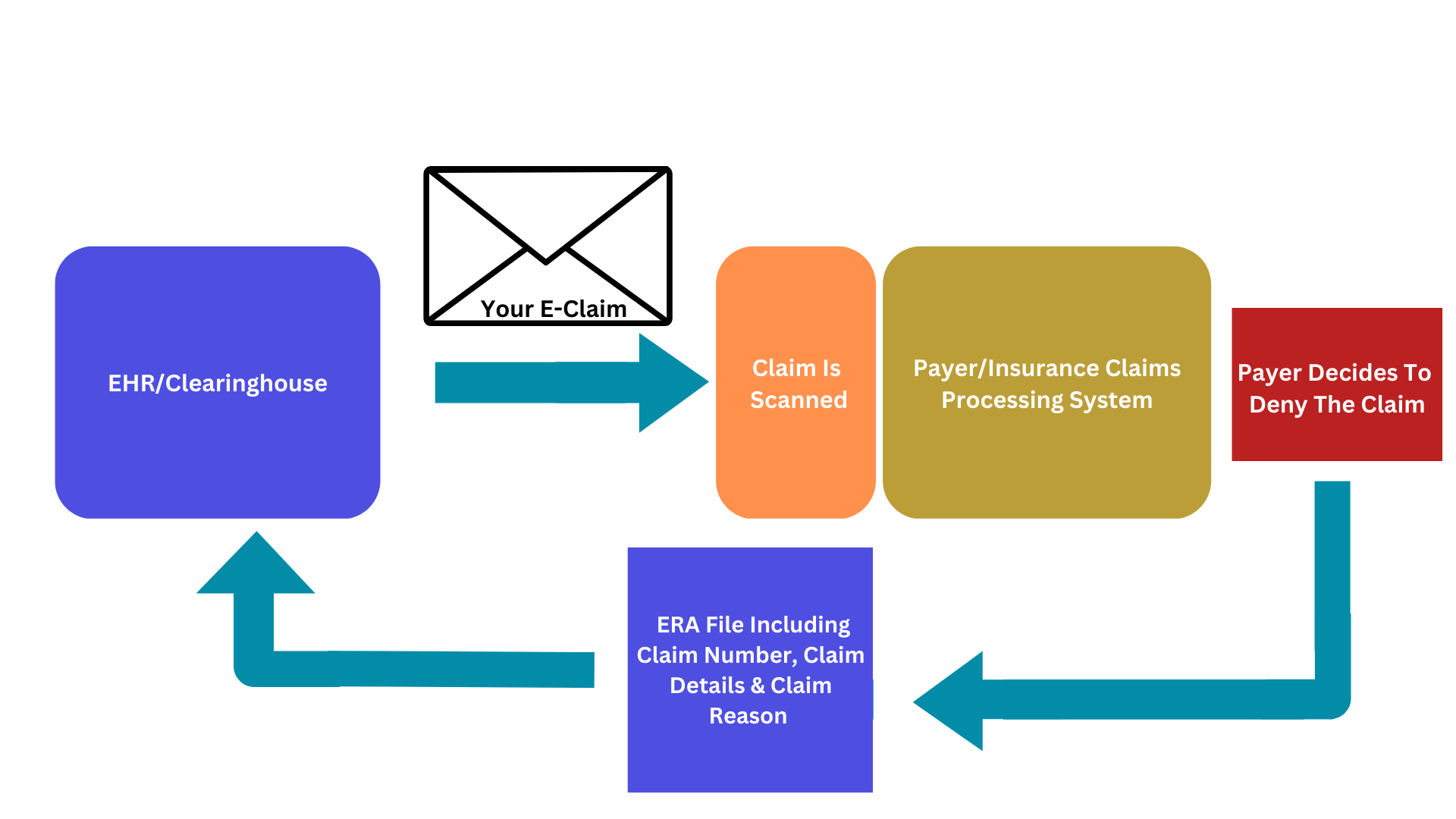
Claim denials are the decision not to pay a claim made by the payer/insurance once the payer’s claims processing system has adjudicated the claim. In the case of a claim denial, the claim was accepted for processing; this means that the claim will have an assigned claim number from the payer, and you can get a claims status update from the payer either online or over the phone. Claim denial details can also be found on ERA (electronic remittance advice) files and EOBs (explanation of benefits). Your EHR system should have a way to accept your payers’ ERA files and display them to you in an easily readable way. Checkpoint EHR also has a section of its software dedicated to displaying ERA files. The system also allows those ERA files to inform other parts of the system so that you can see denials from the clients’ profiles and in reports. Claim denial reasons are often more complex than claim rejection reasons, but they don’t have to be. Some common claim denials that we see are (but certainly are not limited to):
“Precertification/prior authorization absent.”
“Duplicate claim”
“Invalid/missing billing code modifier”
The tricky thing about claim denials is that providers often need to submit a corrected/replacement claim to get a claim paid after it has been denied. Therefore, it is always best to ask the payer if the claim can be resubmitted or if a corrected/replacement claim needs to be submitted to avoid a second claim denial for a “Duplicate claim.” See the graphic above to help you visualize the path of a denied claim.
At Checkpoint EHR, we work to empower mental healthcare providers who use our system to handle their billing issues. Mental healthcare billing can feel daunting, but with an EHR system that makes viewing and reporting on your billing simple and a customer support team to help as much as possible, it can be easier.
Schedule a Checkpoint EHR Demo Today
If you’d like to learn more about the benefits of Checkpoint EHR, reach out to a member of our team today to schedule a demo of our electronic health records software.