Pre-Authorizations and Pre-Claim Reviews for Therapists
Why Therapists Need a Pre-Authorization and Pre-Claim Review Process
For behavioral health therapists who accept insurance, handling claims is an important part of providing good care. One of the most critical processes to ensure timely and accurate reimbursement is pre-authorizations and pre-claim reviews. Without a good system, providers may face claim denials and payment delays. These issues can hurt both practitioners and clients, not to mention lead to financial losses.
In this article, we will cover:
- The difference between pre-authorization and prior authorization
- Who is responsible for managing these processes
- How long they take and when they should be done
- The overall steps required for pre-authorizations and pre-claim reviews
- Best practices for streamlining these essential workflows
What is Pre-Authorization and Prior Authorization?
Pre-Authorization vs. Prior Authorization: What’s the Difference?
Many therapists use the terms pre-authorization and prior authorization interchangeably, but there is a slight distinction:
- Pre-Authorization: This is a general term for getting approval from an insurance company before providing a service.
- Prior Authorization means that someone must check and approve a service before the provider delivers it.
Both terms mean that some behavioral health services need approval from insurers before treatment. This ensures that they receive coverage.
Who is Responsible for Handling Pre-Authorizations and Pre-Claim Reviews?
Managing pre-authorizations and pre-claim reviews usually involves several roles in a behavioral health practice.
- Therapists (especially in solo practices) may need to handle this process themselves.
- Administrative Staff or Billing Specialists in larger practices manage these tasks on behalf of providers.
- Third-Party Billing Companies can take care of pre-authorizations and claim submissions for outsourced billing solutions.
- Electronic Health Record (EHR) Systems like CheckpointEHR can streamline the process of insurance authorization and claim tracking.
How Long Do Pre-Authorizations Take?
The time it takes for pre-authorization varies. The process depends on several factors, such as the insurance provider, service, and the quality of the request. Here’s a general breakdown:
- Standard Pre-Authorizations: Typically processed within 5 to 10 business days.
- Expedited or Urgent Requests: Typically completed within 24 to 72 hours, depending on medical necessity.
- Appeals for Denied Authorizations: May take weeks to months, depending on the insurer’s process.
Since delays can impact client care, therapists should initiate pre-authorizations as early as possible.
When Should Pre-Authorizations Be Done?
Therapists should check for pre-authorization requirements before the first appointment if:
- The client has Medicaid, Medicare, or an HMO plan, which often requires prior authorization.
- The therapy service is for higher levels of care (e.g., intensive outpatient programs, psychological testing).
- The client’s insurance plan requires pre-authorization for mental health services.
Additionally, some insurers require periodic re-authorizations, especially for extended treatment plans.
Steps for the Pre-Authorization Process
1. Verify Client Insurance Coverage
Before providing any therapy session, check the client’s insurance details, including:
- Deductibles and copays
- Out-of-network coverage
- Pre-authorization requirements
- Limits on session frequency or duration
Many EHR systems offer verification checks to streamline this step.
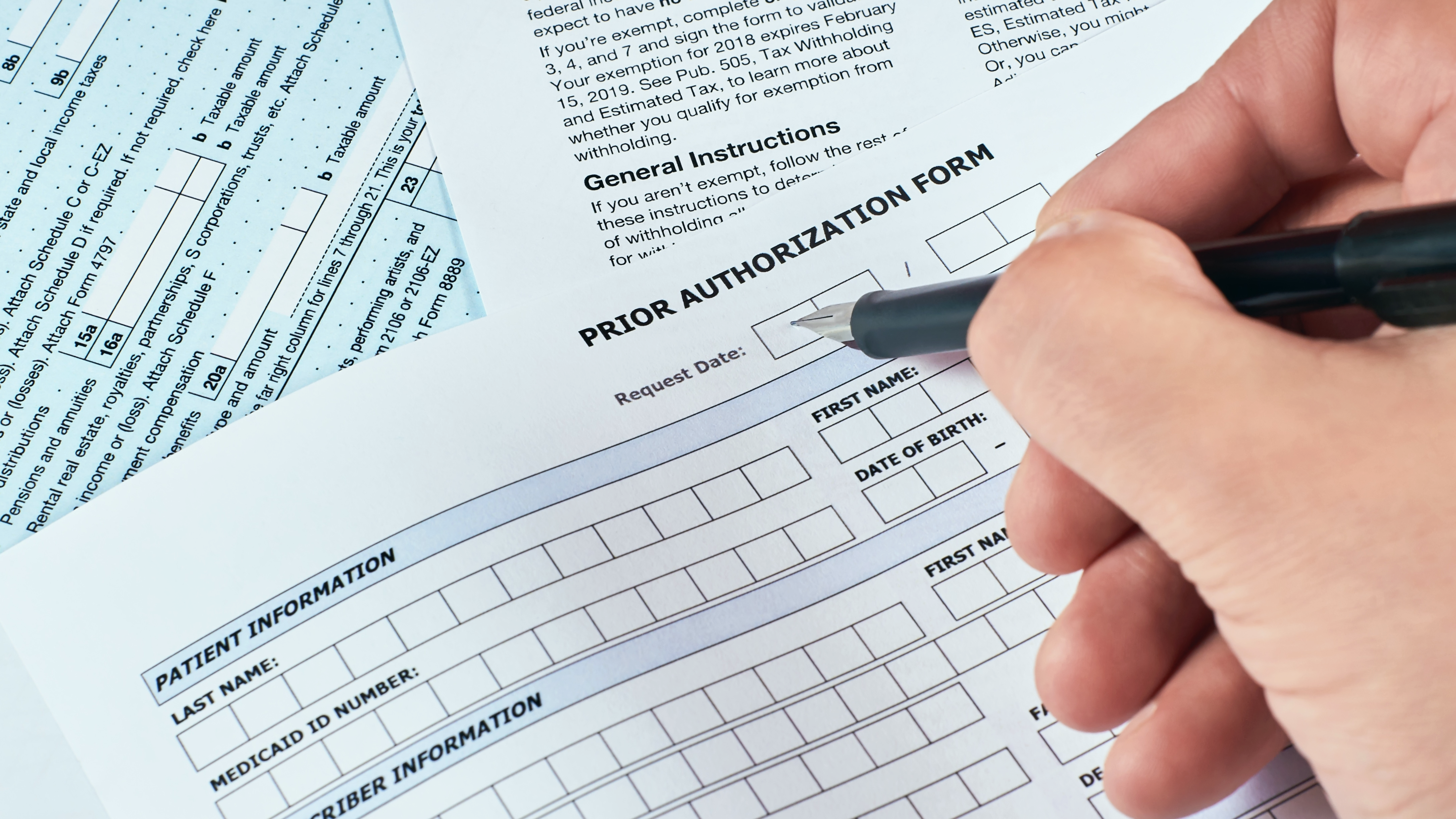
2. Gather Required Documentation
Insurance companies typically require specific information, such as:
- Diagnosis codes (ICD-10)
- CPT codes for the planned services
- Clinical notes supporting medical necessity
- Treatment plans outlining goals and progress
3. Submit the Pre-Authorization Request
Pre-authorizations can be submitted through:
- Insurance provider portals (fastest method)
- Faxed forms (some insurers still require this)
- Phone calls (used for urgent cases)
Some insurers require a peer-to-peer review. In this process, the therapist talks with a reviewer to explain the request.
4. Monitor Approval Status
After submission, it’s important to follow up regularly. Set reminders to check on pending authorizations to avoid delays in care.
5. Notify Clients of Authorization Status
Once approved, inform the client about their coverage, copayments, and any session limits imposed by their plan.
6. Document Approval in EHR System
Record the authorization details, including:
- Approval number
- Authorized services and session limits
- Expiration date
Keeping detailed records will help prevent claim denials.
What is a Pre-Claim Review and Why is it Important?
Pre-Claim Review: Ensuring a Smooth Reimbursement Process
A pre-claim review is the process of reviewing claims before submission to prevent denials and rejections. This ensures:
- Billing accuracy (correct CPT codes, modifiers, and diagnosis codes)
- Compliance with insurance policies
- Avoidance of common claim errors that lead to payment delays
Having a process to prepare for these pre-claim reviews when they happen is important.
Steps for Pre-Claim Reviews
- Verify Service Documentation: Ensure therapy notes match the billed services.
- Check for Authorization Requirements: Confirm that any required approvals are in place.
- Confirm Coding Accuracy: Use the correct CPT and diagnosis codes.
- Ensure Claim Form Completeness: Double-check client details, session dates, and provider information.
- Submit and Track the Claim: Once reviewed, submit the claim through your behavioral health EHR for faster processing.
Best Practices for Streamlining Pre-Authorizations and Pre-Claim Reviews
To reduce administrative burden and improve revenue cycle management, therapists should:
- Use an EHR with integrated billing features to streamline verification checks and pre-authorizations.
- Develop standard workflows for handling authorizations and claim reviews.
- Outsource billing tasks to a specialized provider if in-house management is overwhelming.
- Regularly train staff on the latest insurance guidelines and common claim errors.
For more insights, check out resources like Thrizer’s Guide to Prior Authorizations or Medicaid’s Prior Authorization Initiative. Both resources offer valuable billing, authorization, and claim submission insights.
Conclusion
Having a clear pre-authorization and pre-claim review process is essential for therapists who accept insurance. Without it, claim denials, payment delays, and financial losses can become common issues.
Ultimately, methods such as manual tracking, administrative help, and EHR automation can help optimize revenue. This will lower stress and let you focus more on caring for your clients.
For more support, consider using CheckpointEHR to simplify pre-authorization and billing workflows. Such modern electronic health records can ensure smooth operations and steady cash flow.