A 7-Step Guide to Navigating Mental Health Billing

Mental health billing can be a complex and time-consuming process, but it’s manageable with the right approach. Properly setting up your billing process ensures that providers are fairly compensated while maintaining compliance with various regulations. This guide outlines the key steps involved in mental health billing, offering a clear, step-by-step overview from the initial client contact to managing rejections and appeals.
1. Gather Client Information
The billing process begins by collecting comprehensive client details. This includes personal information such as name, date of birth, address, and contact details. Additionally, it’s essential to gather insurance information, including the insurer’s name, policy number, and group number. Accurate data collection at this stage helps prevent errors later in the billing process.
2. Verify Client Information and Eligibility
Once client information is collected, the next step is to verify the details and check insurance eligibility. This involves confirming that the client’s insurance is active and that the services to be provided are covered under their plan. Verification can be done through online insurance portals or by contacting the insurance provider directly. Some EHRs and clearinghouses also offer automated eligibility checks. Ensuring eligibility upfront minimizes the risk of claim denials due to inactive policies or non-covered services.
3. Record the Appropriate CPT Code(s)
Accurate recording of Current Procedural Terminology (CPT) codes is crucial for precise billing. CPT codes are standardized codes used to describe the procedures and services provided during a client’s session. Each code corresponds to a specific service, such as individual therapy, group therapy, or psychiatric evaluation. Proper CPT coding ensures claims are processed correctly and providers are reimbursed appropriately.
4. Submit Claims
After verifying client information and recording CPT codes, the next step is to submit the claim to the insurance company. Claims can be submitted electronically or on paper, though electronic submission is generally quicker and more efficient. The claim should include all necessary details about the client, provider, and services rendered. Ensuring all information is complete and accurate at this stage is crucial to avoid processing delays.
5. Handle Clearinghouse Rejections
Once a claim is submitted, it often goes through a clearinghouse, which reviews the claim for errors before forwarding it to the insurance company. Clearinghouses check for issues such as incomplete information, incorrect CPT codes, and eligibility problems. If a claim is rejected by the clearinghouse, it must be corrected and resubmitted. Promptly addressing these rejections can significantly streamline the billing process and prevent delays in provider compensation.
6. Process Claims
After passing through the clearinghouse, the insurance company processes the claim. This involves reviewing the claim to ensure it meets all requirements and determining the reimbursement amount. Providers receive feedback via an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA), detailing how the claim was processed, the amount paid, and any reasons for partial payment or denial.
7. Review Denials and Record, Rework, or Appeal
Despite best efforts, some claims may be denied. Common reasons for denial include incorrect client information, non-covered services, and coding errors. It’s essential to review and record all denials thoroughly. Understanding why a claim was denied is the first step in addressing and correcting the issue. Providers can then rework and resubmit the claim after correcting any errors. If a claim is denied for reasons such as medical necessity, providers can appeal the decision with additional supporting documentation. Persistence in reworking and appealing denied claims can significantly impact a practice’s revenue.
Choosing the Right Clearinghouse
The effectiveness of your mental health billing process is significantly influenced by selecting the clearinghouse and billing service that best serves your clinic or agency. Here are some frequently referenced clearinghouses:
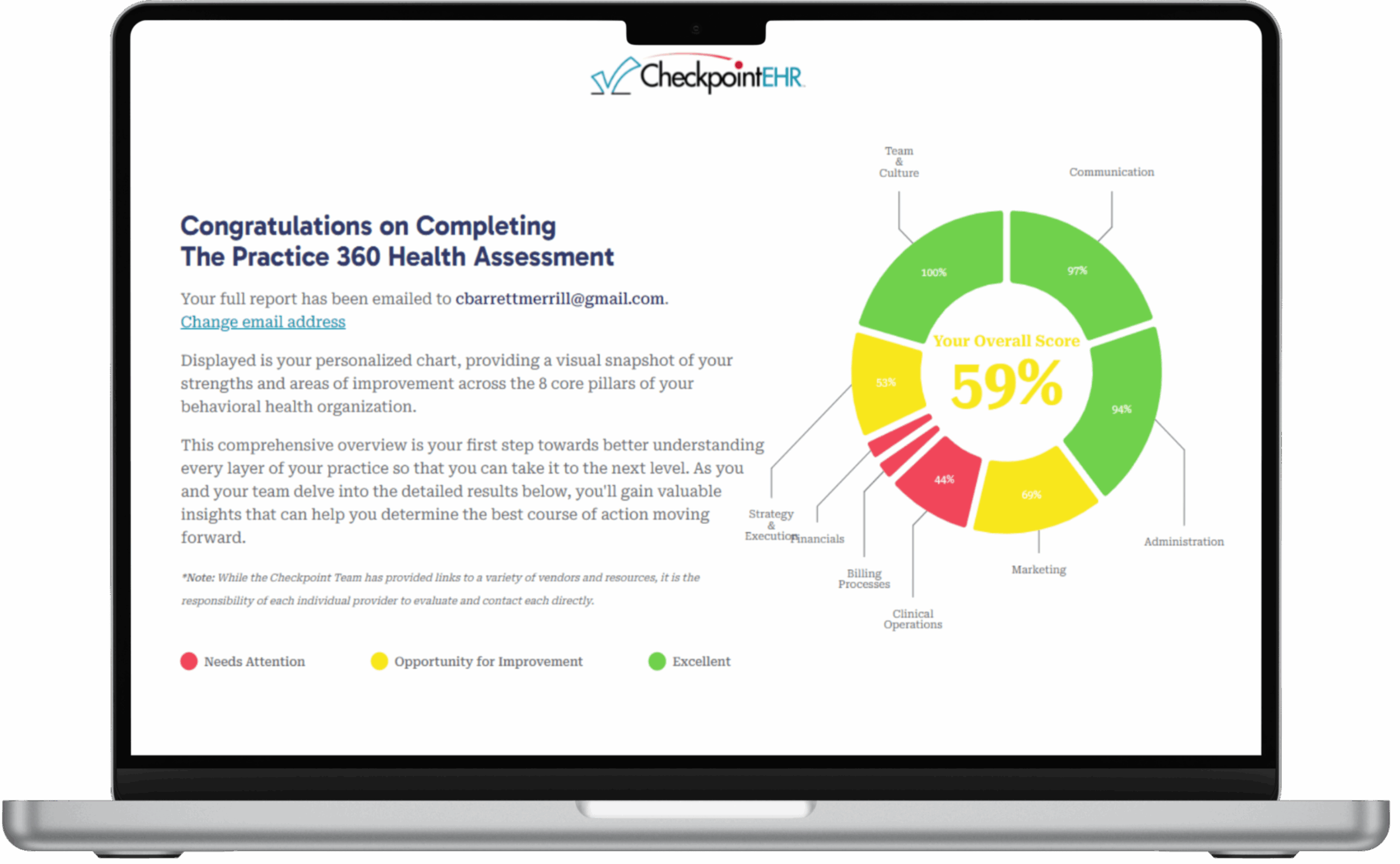
And, of course, our personal favorite, Availity, an integrated partner of ours here at Checkpoint EHR. This partnership enables us to offer a hands-free billing experience, accelerating the billing process, maximizing reimbursements, and handling clearinghouse tasks so our therapists can focus on their top priority: their clients
Learn How We Can Help You Today