AI-Assisted Notes: The Benefits & Cautions
by CheckpointEHR, in collaboration with Upheal
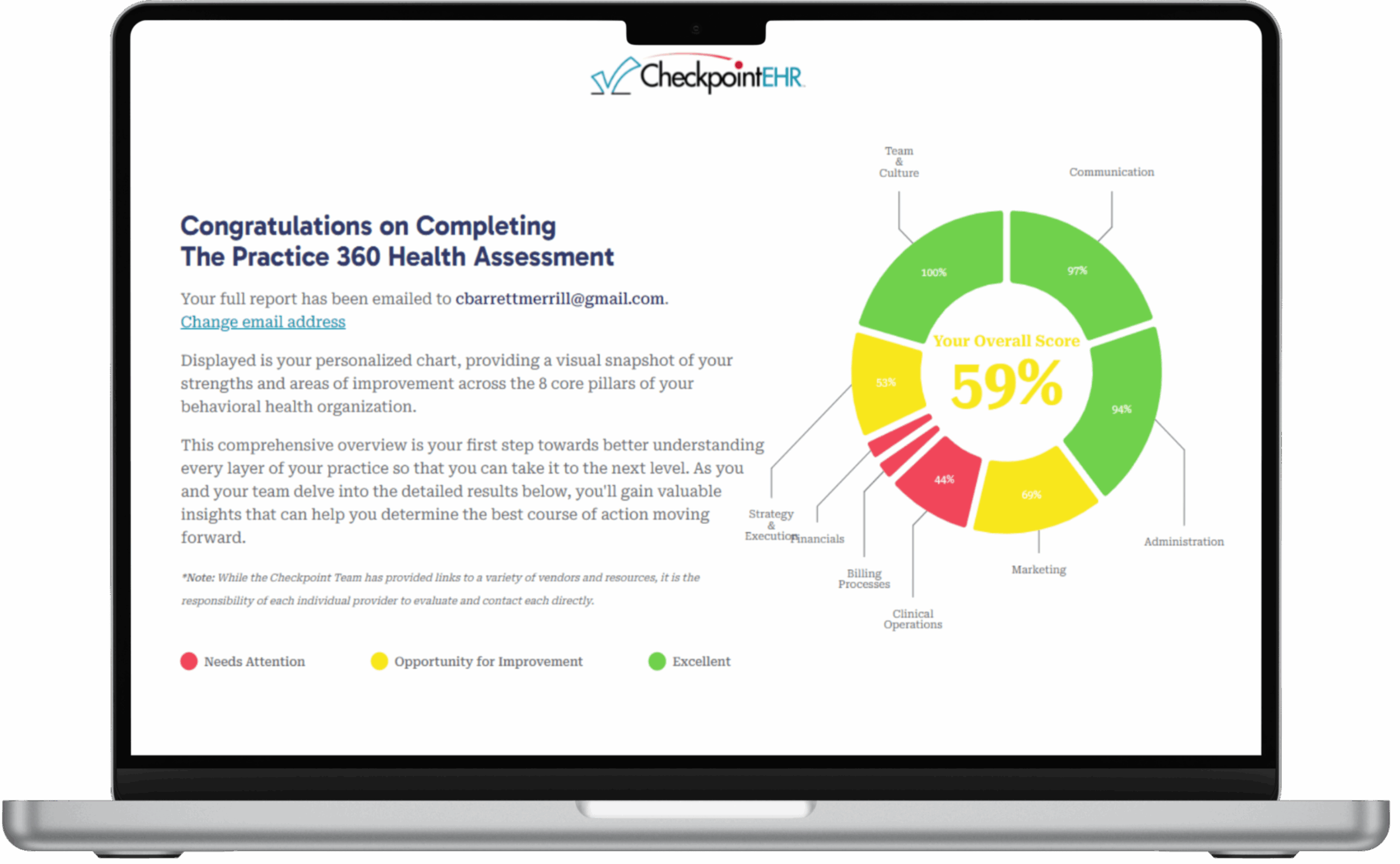
In a profession where documentation is essential—but often overwhelming—the idea of using artificial intelligence (AI) to assist with progress notes has moved from science fiction to real-world solution. At CheckpointEHR, we’re always looking for ways to help behavioral health professionals work more efficiently and sustainably. That’s why we’re excited to highlight the potential of trusted AI-assisted notes tools like Upheal. Such platforms are setting the bar for clinical-grade, ethical, and secure AI documentation support among mental health therapists.
Let’s explore what AI-assisted notes are (and aren’t), how they can save you time and improve your clinical documentation, and what to be mindful of as you explore integrating these powerful tool into your practice.
What Are AI-Assisted Notes?
AI-assisted notes are a form of digital documentation support that uses artificial intelligence—specifically natural language processing (NLP) and machine learning—to transcribe sessions and generate drafts of clinical documentation, such as progress notes (e.g. SOAP note), session summaries, and even treatment plans.
Platforms like Upheal document your sessions (with consent), transcribe the audio, identify key clinical markers (e.g., symptoms, goals, interventions), and then create draft notes that align with common documentation standards, such as SOAP, DAP, or BIRP.
Importantly, AI-assisted notes are not fully autonomous documentation.
You are still the author and clinical decision-maker. AI doesn’t diagnose, treat, or replace clinical judgment—it assists, expedites, and supports the process (with your guidance) by synthesizing information so that you can focus more on your client and less on your keyboard.
Safety and Security First: What You Need to Know
We know that privacy is paramount in our field. That’s why security and compliance must come first when evaluating any AI documentation tool. Nothing is more important when evaluating new mental health technologies than protecting health information.
For instance, Upheal’s platform is HIPAA-compliant, SOC2 certified, and designed with end-to-end encryption. They’ve taken the essential steps to ensure client data is protected at every point—during storage, in transit, and when clinical notes are generated.
When integrating AI into your documentation workflow, always ensure the product you use complies with your region’s privacy and security regulations and that it offers the transparency and control you need to maintain client trust and ethical standards.
The Benefits: Time Savings and Better Notes
If you’ve ever found yourself finishing session notes long after your last client has gone home—or worse, logging in on the weekend to catch up—you’re not alone.
According to Upheal’s internal data, therapists using their platform report an average of 1–2 hours saved per day, with many reducing documentation time by over 50%.
But the benefits go beyond just efficiency:
1. More Present, Less Distracted
With the confidence that a draft will be ready after session, you can be more attuned to your client in real time. No more glancing at the clock or scribbling frantically—AI is listening with you.
2. Higher Quality Notes
AI-generated notes can include objective language, consistent formatting, and structured summaries that are easy to review and audit. Some tools even help align your mental health notes with treatment goals and insurance requirements. In addition, AI-assisted notes can progressively support new clinicians in learning how to craft higher quality notes.
3. Faster Treatment Planning
By pulling forward themes, goals, and progress markers, AI tools can support the creation of treatment plans with greater clarity and alignment—without starting from scratch.
4. Support for Group Practices
For practices managing multiple clinicians, AI-assisted notes can promote consistency and reduce administrative oversight by standardizing note structure and quality across providers.
What to Be Cautious About
While AI-assisted documentation is an exciting advancement, it’s not without risks or considerations. Here are a few important cautions to keep in mind:
1. You’re Still the Clinician
AI can identify key themes, but it can’t assess nuance the way you do. Always review, edit, and approve notes carefully to ensure they reflect your clinical judgment and voice.
2. Informed Consent is Critical
Clients need to know their sessions may be recorded, transcribed, or analyzed. Tools like Upheal provide client consent templates and secure workflows, but it’s your responsibility to ensure clients are informed and comfortable.
3. Avoid Over-Reliance
If you begin to rely too heavily on AI outputs without critically engaging, your clinical documentation may become generic or lose its depth. AI should assist—not replace—your thoughtful reflection on the client’s progress.
4. Check Alignment with Payers
For those billing insurance or Medicaid, ensure your AI-generated notes meet documentation requirements. The good news is, platforms like Upheal are designed with payer expectations in mind—but again, you’re the final reviewer.
Tips for Incorporating AI-Notes Effectively
Adopting new technology takes more than signing up for a platform. It requires the right mindset and strategy. Here’s how to get started thoughtfully:
✅ Start Small
Try AI-assisted notes with a few clients first, especially those that will be most comfortable with early consent. Notice how the workflow impacts your time, energy, and quality of documentation before rolling it out more broadly.
✅ Use It to Enhance, Not Replace
Think of AI as a second brain—it helps you synthesize, but your insight is still the engine behind great care. Consider using the AI drafts as a first draft, then personalize as needed.
✅ Maintain Client-Centered Ethics
Revisit your informed consent processes, consider how clients might feel about recording sessions, and be transparent about why you’re using AI and how it benefits their care.
✅ Review Regularly
Periodically assess the quality and accuracy of your AI-generated notes. Are they helping? Are they introducing any blind spots? Stay engaged in the process.
A New Era of Documentation
At CheckpointEHR, we understand that running a behavioral health practice isn’t just about good systems—it’s about sustainable care. That includes making documentation less burdensome, without compromising quality or ethics.
Upheal’s AI-powered documentation assistant is one of the most promising tools we’ve seen in this space, with features designed specifically for mental health providers, thoughtful consent workflows, and a deep commitment to privacy and security.
If you’re curious about AI-assisted progress notes as a behavioral health provider but cautious about the implications—good. You should be. This technology is powerful, and with power comes responsibility. But with the right guardrails, mindset, and partners, AI can truly help behavioral health therapists reclaim their time, improve their notes, and focus more deeply on what matters most: the people they serve.
Ready to explore how AI-assisted notes could transform your documentation process?
Learn more about Upheal’s secure, clinician-friendly platform here. You might just find it’s the extra set of (virtual) hands you didn’t know you needed.
Looking for a modern and intuitive behavioral health EHR system to streamline documentation for your practice—CheckpointEHR is here to support you every step of the way.