What Therapists Need to Know About the CMS-1500

For behavioral health therapists accepting Medicaid, one of the most critical documents for submitting claims is the CMS-1500 form. This standardized form is essential for tracking services and getting paid for care that’s been provided. Here’s what you need to know about it.
Who Uses the CMS-1500 Form?
The CMS-1500 form, also known as the “Health Insurance Claim Form,” is used by healthcare providers, including therapists, to bill insurance companies for outpatient services. It’s primarily utilized by non-institutional providers, such as private practice therapists, group practices, and outpatient clinics. If you’re a behavioral health professional submitting claims to Medicare, Medicaid, or private insurance companies, the CMS-1500 form is likely your go-to billing tool. Learn more about CMS-1500 from the Centers for Medicare & Medicaid Services (CMS).
What Does the CMS-1500 Form Include?
The CMS-1500 form captures detailed information about the behavioral health services you provide, along with vital client and provider information. It includes:
- Patient Information: Name, address, date of birth, and insurance details.
- Provider Information: Your name, address, National Provider Identifier (NPI), and Tax Identification Number (TIN).
- Service Details:
- Dates of service.
- Place of service codes (e.g., 11 for office visits, 02 for telehealth).
- Current Procedural Terminology (CPT) codes for the services rendered.
- Diagnosis codes (ICD-10).
- Billing Information:
- Total charges.
- Amount paid by the patient.
- Insurance information, including the policyholder’s details.
- Signature and Authorization: Attestation from the provider and, if necessary, the patient.
When and How to Fill Out the CMS-1500 Form
You’ll typically complete and submit a CMS-1500 form after a session or a set of sessions, depending on your billing cycle. Here’s a step-by-step guide to ensure accuracy:
- Obtain Accurate Patient Information: Before services begin, gather and verify the patient’s insurance details and personal information. Errors in this data can delay reimbursement.
- Code Services Correctly:
- Use appropriate CPT codes to describe the therapy sessions. Explore CPT codes on the American Medical Association (AMA) website.
- Match ICD-10 diagnosis codes to justify the services. Find ICD-10 resources from CMS.
- Include All Necessary Details: Double-check that every field on the form is complete. Missing information can lead to claim rejections.
- Submit Electronically or by Mail:
- Many providers use electronic health record (EHR) systems, like CheckpointEHR, to generate and submit CMS-1500 forms electronically. This method is faster and reduces errors.
- Alternatively, you can print and mail paper forms to the insurance company’s claims processing address.
What Happens If It’s Filled Out Incorrectly?
Errors on the CMS-1500 form can result in claim denials, delayed payments, or audits. Common mistakes include:
- Incorrect Patient Information: Mismatches between the patient’s name and insurance details can lead to rejection.
- Coding Errors: Using outdated or incorrect CPT or ICD-10 codes may result in denials.
- Incomplete Fields: Missing provider signatures, service dates, or other required fields can halt claim processing.
- Submission Errors: Submitting the claim to the wrong payer or using an outdated form version can cause delays.
If your claim is denied, the insurance company will typically provide an explanation of benefits (EOB) detailing the reason. Correct the errors promptly and resubmit the form.
Why Accuracy Matters
Filling out the CMS-1500 form accurately is not just about getting paid on time; it’s also a matter of compliance. Incorrect or fraudulent claims can result in:
- Audits by insurance companies or government agencies.
- Fines or penalties for non-compliance.
- Damage to your professional reputation.
Tips for Streamlining the Process
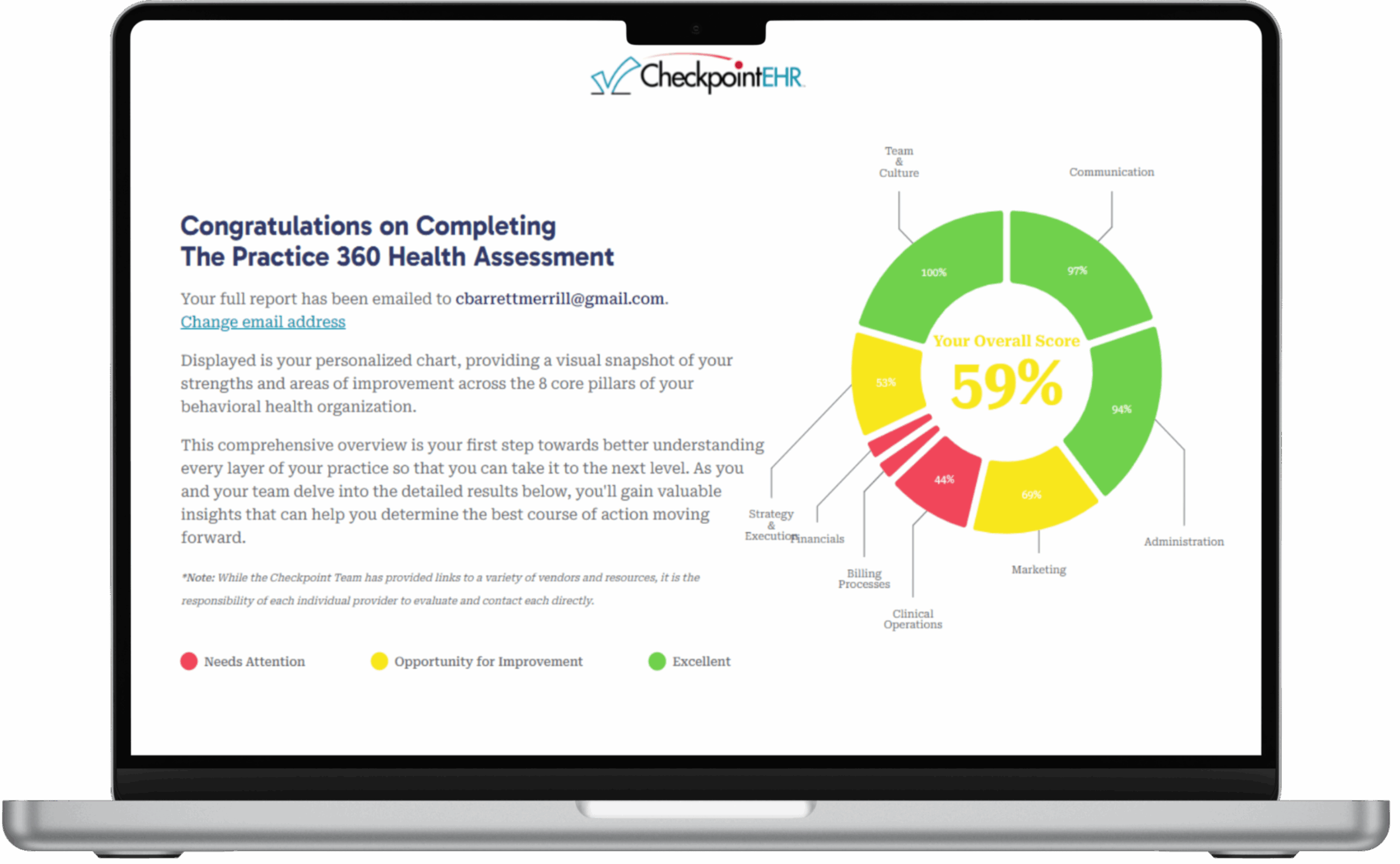
- Invest in an EHR System: Using an EHR like CheckpointEHR can automate a large portion of the claim submission process, reducing errors and saving time.
- Stay Updated on Coding Standards: CPT and ICD-10 codes are updated annually. Ensure you’re using the most current versions. [Visit the AMA and CDC websites for updates.]
- Train Your Staff: If you have administrative support, ensure they’re well-versed in billing procedures.
- Verify Insurance Coverage Before Services: Check patient eligibility and benefits to avoid surprises.
- Keep Accurate Records: Maintain thorough documentation of all sessions and communications with patients and insurers.
Conclusion
Understanding and mastering the CMS-1500 form is essential for therapists who bill insurance companies. While it may seem complex initially, proper training, attention to detail, and the right tools can simplify the process. By ensuring accuracy and compliance, you can focus more on providing exceptional care and less on administrative headaches.