Epic Systems Corporation Accused Of Fraud

Epic Systems Corporation a leading EHR system provider, is facing a lawsuit that alleges its system fraudulently bills Medicare and Medicaid more than it should for anesthesia services.1
The lawsuit was initiated by Geraldine Petrowski, a former employee of WakeMed Health in Raleigh, North Carolina, under the False Claims Act. The terms of the act mean lawsuits filed under the False Claims Act are kept sealed while the fraud investigation is carried out.
That investigation has now been completed, so the lawsuit details have been unsealed.
Epic has denied any wrongdoing. Epic spokesperson Meghan Roh claims Petrowski´s claims are based on a misunderstanding of how the system is intended to work.2 Roh points out that the Department of Justice has decided to take no further action, although that is not the end of the case.
Errors in Anesthesia Billing
The case hinges on the fact that the Epic system allows users to charge for anesthesia services using both units and minutes, instead of confining any given bill to one or the other. This can result in inflated claims being entered for these services.
While it is clear that the system does allow this, and there is little doubt that incorrect claims have been submitted, there is still considerable doubt as to whether Epic can be found guilty of fraudulent behavior.
The Epic system does not force users to issue inflated bills. It would seem likely that Epic will defend itself by alleging that any fraudulent activity occurs at user level and not at system level. The court case is likely to drag on for years. If found guilty, Epic could face massive fines for every incident of overcharging. Even if Epic successfully defends the lawsuit, it is likely to suffer damage to the organization’s reputation.
The problems that Epic faces could be faced by any healthcare provider who submits Medicaid or Medicare claims that are inaccurate. The chances of submitting bad claims or inadvertently fraudulent ones are much higher for healthcare providers who manage their own medical billing.
Errors Cost Money
Errors are common occurrences. Provided there is no intention to defraud, there will be no legal penalty for making errors. This does not mean that errors do not have a cost implication.
When claims are submitted for payment, they are checked for accuracy before payment is issued. If any problems are detected, the claim is rejected. The errors must be fixed, the claim resubmitted and the whole process repeated.
This is time-consuming and involves staff duplicating work, which comes with a cost penalty. The effect on turnover also has a cost implication.
Avoiding Errors on Claims
Many providers are aware of the potential for submitting incorrect claims. However, the cost of using third-party claims processing is often prohibitive, forcing them to take the risk of making incorrect claims.
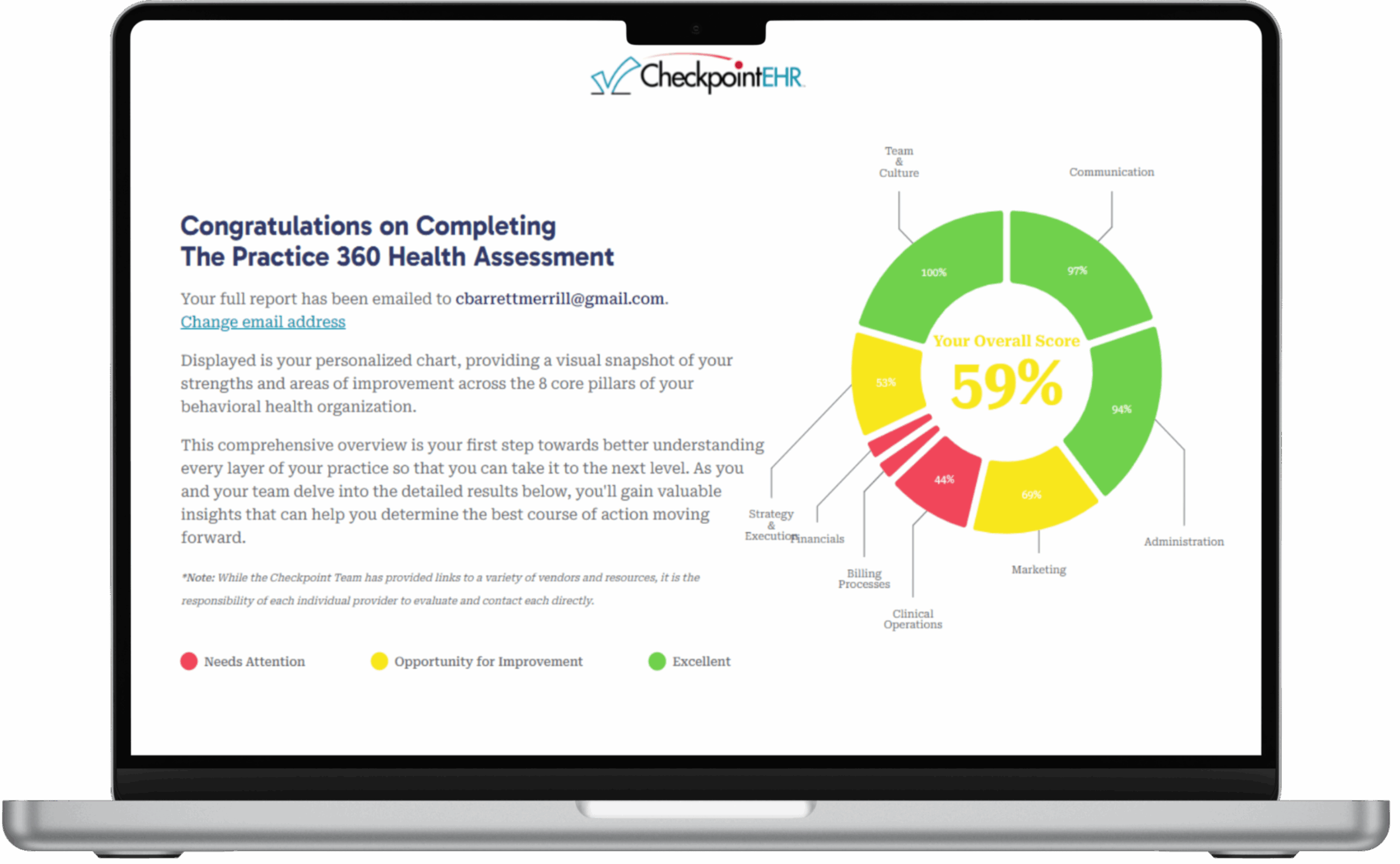
There is a solution to this problem. Checkpoint EHR has a revenue-based billing model that includes clearinghouse fees.2 This is a very cost-effective way for a business to effectively outsource its medical billing. It also reduces costs incurred through incorrect claims. It should also protect a provider from the type of legal claim issued against Epic.