Is Third-Party Mental Health Billing Worth the Cost?

At first glance, mental health billing assistance would seem to be a wise investment for behavioral health providers. It removes the overhead associated with in-house billing. However, determining whether it is the right option for a particular healthcare provider requires a certain amount of analysis.
In some cases, it will undoubtedly be the best option, while in others, keeping the billing function in-house will prove to be the better option. A cost-benefit analysis should be undertaken before any decision is reached.1
Direct Costs of Mental Health Billing Assistance
While billing fees vary between service providers, the most widely used model involves the billing assistance service provider charging a percentage of the fees collected. Some service providers will charge a baseline fee that must be paid regardless of how much is collected from mental health bills. This model makes it tricky to forecast the amount that will be paid in fees, but it should be possible to arrive at a reasonably accurate processing cost.
It is also necessary to factor in the in-house costs that will still accrue even when third-party mental health billing assistance is used. These will include hardware and software. Busier healthcare providers may need to recruit one or more dedicated secretarial staff to compile and send data to the medical billing assistance provider.
Costs of In-House Billing
All but the smallest behavioral health providers will most likely need to employ someone to manage the medical billing process. This function is best allocated to a person who is fully trained in mental health billing. Trying to perform mental health billing using other, unspecialized clerical staff will most likely result in significant errors and inefficiencies.
Medical billing and coding is quite complex, and inexperienced billers are prone to making mistakes. These errors can result in claims being denied and services being undercharged, and a lot of time can be wasted correcting errors. That is why it is essential to use certified coders, and these obviously come at a cost.
Mental health coding is a dynamic entity, with codes being added and removed frequently.2 Since a practice using in-house billing will be entirely reliant on specialist staff, it will need to invest in ongoing training. The practice will also need to have a system in place to cover for billing staff being out of the office with a sick day or vacation time.
Indirect Costs of In-House Billing
When assessing the benefits of in-house billing compared with using mental health billing assistance, the most significant indirect costs arise when the task of in-house billing is not allocated to specialist staff. This is an area that is frequently overlooked by healthcare providers. Smaller practices may be tempted to allocate the mental health billing function to one or more existing staff members, which could even include clinical staff.
However, when clinical staff are diverted from doing the work for which they are qualified, that has an impact on the earning potential of a practice. For example, any doctor who needs to spend time on billing cannot see as many patients as one who is not doing essentially secretarial work. This loss of income represents an indirect cost.
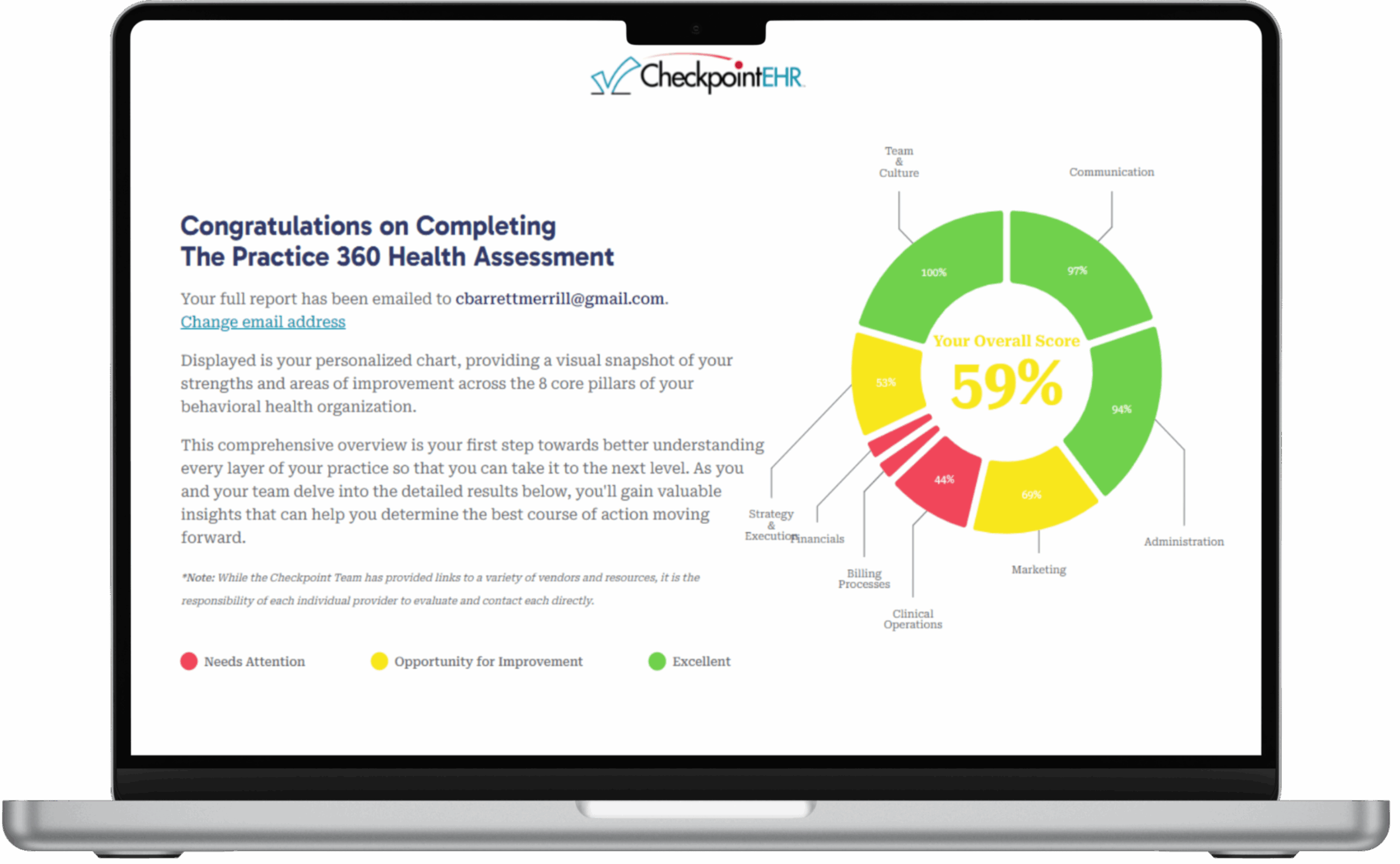
One way to make the decision to opt for medical billing assistance easier is to choose an EHR system, such as Checkpoint EHR, in which the billing function is included in the cost of the EHR. That can make the difference between medical billing assistance being profitable rather than being just an additional overhead.